The publication of the
succinctly titled;
‘International
framework for examination of the cervical region for potential of Cervical
Arterial Dysfunction prior to Orthopaedic Manual Therapy intervention’
(Rushton, et al 2013)
... has highlighted the need for manual therapy clinicians to
be cognisant with cervical arterial
dysfunction (CAD).
BUT what is that? … and what does it
mean to clinicians?
Let
us start ... by dealing with what it is NOT
 |
| Dissection of an artery |
- Cervical arterial dysfunction is NOT cervical
arterial dissection! That may seem obvious to some, but both acronyms are now
in common usage and therefore some confusion may arise. The term dissection is specific to dissection
events (see image) and therefore narrow. Cervical arterial dysfunction is a broader term which is all-encompassing of a range of
pathologies which may affect the cervico-cranial vasculature.
- CAD is NOT vertebro-basilar insufficiency
(VBI). However, it does incorporate it - as one of the component parts of a wider
system based approach to thinking about haemodynamics and ischaemia
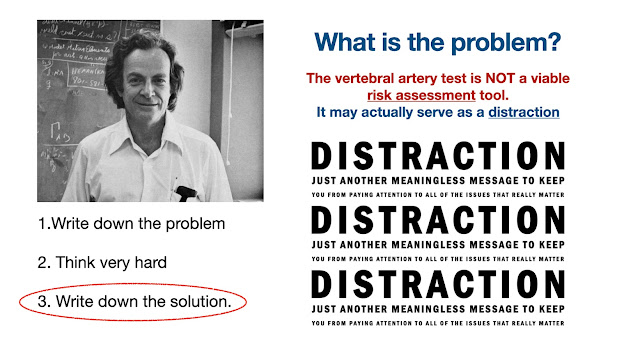
- Above all, CAD is NOT (in isolation) dissection of the
vertebral artery. That would simply be a continuation of the narrow thought process
which lead us to believe that a single test i.e. the vertebral artery test,
could somehow allow us to decide whether cervical manipulation was ‘safe’ or
not! That outdated concept has thankfully been de-bunked once and for all, as
we move closer to science based practice.
So what is cervical arterial dysfunction
then…?
CAD is a consideration of ALL of the potential arterial
dysfunctions, which may present to, or ensue from a manual therapy
intervention.
CAD
is simply a way of thinking about an age old problem in a different way, and
more importantly asking ourselves different questions about this familiar
problem – linked to RISK and cervical spine management. The emphasis has moved
firmly away from just ‘manipulation’, into a consideration of movement per se.
This clearly widens the thinking into a consideration of ASSESSMENT (which
incorporates movement) as well as intervention, which may incorporate ANY form
of manual therapy or exercise prescription. This is then combined with a consideration of ALL of the potential structures and vascular 'dysfunctions'. Thinking is no longer constrained by one structure or pathology.
So why the shift from VBI and
vertebral artery dissection …?
 Well
first of all, there is a lot more to the cervical vasculature than the vertebro-basilar
system and there is a lot more to the range of pathologies than just dissection.
Dissection or damage to the intimal wall of a vessel is a commonly cited
vascular ‘injury’ thought to be associated with cervical spine manipulation in
particular. However, an understanding of the basic science of haemodynamics
allows us to incorporate many more conditions and pathologies into the paradigm.
Well
first of all, there is a lot more to the cervical vasculature than the vertebro-basilar
system and there is a lot more to the range of pathologies than just dissection.
Dissection or damage to the intimal wall of a vessel is a commonly cited
vascular ‘injury’ thought to be associated with cervical spine manipulation in
particular. However, an understanding of the basic science of haemodynamics
allows us to incorporate many more conditions and pathologies into the paradigm.
There are a range of reasons why blood vessels may be compromised in the
cervico-cranial region, from pre-existing underlying anatomical anomalies, vasospasm,
atherosclerotic disease, through to arteritis (i.e. temporal). All of these may lead
in different ways, to potential ischaemia which may manifest and a variety of
ways, ranging from PAIN, through to blindness, stroke or at worst death.
Some direction for clinicians:

- Develop an understanding that
there is more to cervical spine risk assessment than a consideration of ‘VBI’
or dissection of the vertebral artery.
- Consider a ‘systems based’ approach,
incorporating the whole cervical vascular system, including the carotid vasculature
(and branches) and the whole range of potential pathologies (NOT just
dissection).
- Develop awareness, that whilst
commonly cited vascular risk factors have not been shown to be associated with
dissection pathologies, they are strongly
correlated with atherosclerosis, hypertension and stroke … This is ‘system
based thinking’.
- Develop increased awareness that
neck pain and headache may be the early signs of pre-existing vascular
dysfunction.
- Develop an index of suspicion for
cervico-cranial vascular pathology, particularly in cases of acute trauma or non-resolving/worsening
conditions.
- Enhance subjective/objective
examination by including vascular risk factors such as hypertension, and
procedures such as blood pressure, cranial nerve testing and eye examination.
- Consider carefully the ORDER of
your examination in the presence of potential vascular ‘red flags’.
- Expand manual therapy teaching and
practice to include haemodynamic principals and their relationship to movement,
handling, anatomy and biomechanics.

Despite all this … when all is said and done, the 64m dollar
question still seems to be … Should clinicians perform a ‘vertebral artery
test’?
Answer … there is little to support it's use as a stand alone test. Its sensitivity and
specificity are very poor AND its clinical utility is of little value. It has been argued that it should be retained from a 'medico-legal' perspective, but that contention would most likely be destroyed by any half competent barrister.
Note - that cranial nerve and blood
pressure testing are additional objective measures to incorporate into the physical examination. Both feature prominently in the IFOMPT framework.
For a more detailed
description of this paradigm change see:
‘International framework for examination
of the cervical region for potential of Cervical Arterial Dysfunction prior to
Orthopaedic Manual Therapy intervention’ (Rushton, et al 2013)