That old chestnut the 'vertebral artery test' has been with us in Physiotherapy for nearly 4 decades, and yet still the arguments rage on about its clinical use.
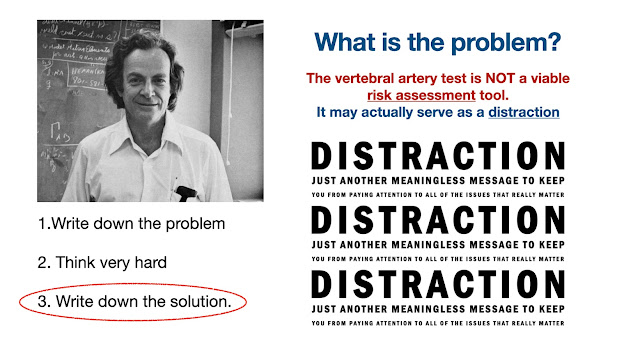
Confusion is never helpful in a clinical (or any) situation, so I've tried to make sense of the background, the logic and ongoing discussion regarding the use of 'the test that refused to die'.
Inspired by the recent debates within the literature, I've put together 3 SHORT FILMS.
Film I, discusses the history of the development and early use of the test. Film II uses some case studies to test the test, and then Film III, takes to the graveyard of old worn out tests, and attempts to offer some logical directions for the future for ALL clinicians working with neck pain, headache, dizziness and visual disturbances.
The key message, is that risk assessment of the cervical spine is relevant for ALL clinicians and NOT (as previously suggested) just for those who practice manual therapy.
What we know from medico-legal cases is that delays to diagnosis and appropriate management can occur for a range of reasons. It may focus the mind to know that some medico-legal cases I've worked on, have involved assessment of the cervical spine (without intervention).
Hopefully, these films and the case studies contained within them will help to guide clinicians with their problem solving and clinical reasoning, in the quest for safe and efficient practice.
I. The Vertebral Artery Test - A SHORT FILM (Part I)
A short educational film about the long and tortuous history of the 'vertebral artery test', of interest to any clinician who manages patients with cervical spine issues.